At-home melanoma testing: Skin patch test works in mice
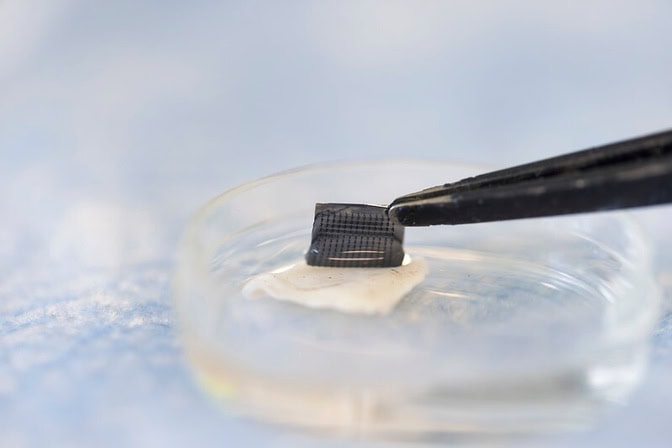
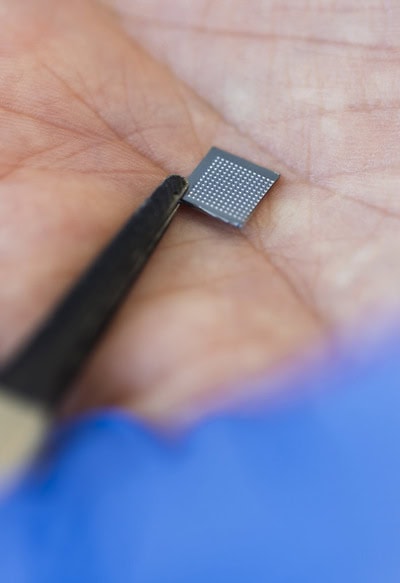
A microneedle patch captures cancer biomarkers in the top-most layer of skin to detect melanoma in animal tissue samples.
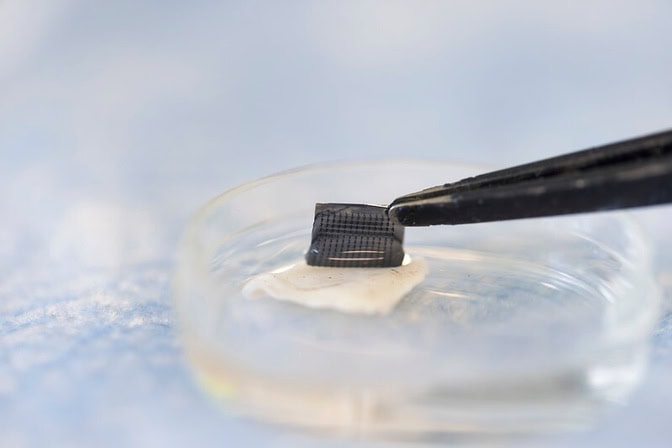
A microneedle patch captures cancer biomarkers in the top-most layer of skin to detect melanoma in animal tissue samples.
Experts
Doctoral Student of Chemical Engineering
Melanoma testing could one day be done at home with a skin patch and test strip with two lines, similar to COVID-19 home tests, according to University of Michigan researchers.
Developed with funding from the National Institutes of Health, the new silicone patch with star-shaped microneedles, called the ExoPatch, distinguished melanoma from healthy skin in mice.
The patch and test move toward rapid at-home melanoma testing, helping patients catch the most aggressive form of skin cancer early without a biopsy or blood draw.
“The star-shaped needles make puncture easier and less painful, but they are so small that they only go through the top-most layer of the skin, the epidermis, and do not draw blood,” said Sunitha Nagrath, the Dwight F. Benton Professor of Chemical Engineering at U-M and co-corresponding author of the study published in Biosensors and Bioelectronics.
Text on screen: This tiny patch could detect signs of skin cancer within 15 minutes. Designed by U-M Engineering researchers, this non-invasive method that proved successful in mice could detect melanoma in the early stages. And it could be performed at home, without the need to visit a clinic. It’s made of microneedles that press into the surface of the skin. The needles are coated in a gel that attracts and binds to cancer indicators within the top-most layer of the skin. It’s then put in a solution and applied to a test strip which will reveal a positive or negative result. Next up, the researchers are planning to move into human clinical trials.
The ExoPatch microneedles, at just 0.6 mm long with a width of less than 100 nanometers (0.0001 mm) at the tip, are coated with a gel that picks up exosomes—tiny packages released by cells—from the interstitial fluid that fills the spaces between cells in the epidermis.
Once thought to be trash ejected from cells for cleanup, exosomes actually contain DNA and RNA fragments that cells use to communicate with each other. Cancer cell exosomes can help tumors spread by preparing tissues to accept tumor cells before arrival, and detecting them can catch cancer earlier than past methods.
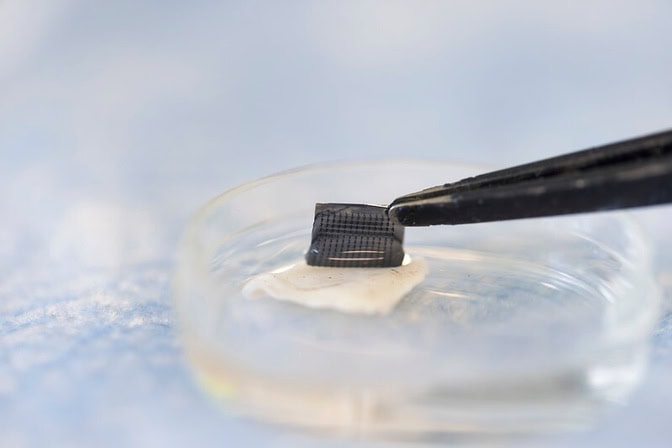
The gel that coats the ExoPatch contains a protein called Annexin V that attracts and sticks exosomes to the microneedles’ surface. Once removed from the skin, placing the patch in an acid dissolves the gel, which releases the exosomes into a solution. After dipping a test strip into the solution, two lines form if the sample contains melanoma exosomes, and one line forms for a negative test—the same way an at-home COVID-19 test strip works.
“A fair-skinned person with moles must go to the doctor about every six months to send off a biopsy to see if they’re malignant or benign. With this test, they could instead test at home, get the results right away and follow up with a dermatologist for a positive result,” Nagrath said.
As a first step in the proof-of-concept study, the researchers tested the ExoPatch on a tissue sample of pig skin, which closely resembles human skin in thickness and composition. Using a microscope, they found the microneedles penetrated about 350 to 600 nanometers into the skin. For scale, the epidermis on the human forearm is about 18,300 nanometers thick.
To test whether the ExoPatch could capture melanoma exosomes from skin tissue, the research team tested tissue samples of mouse skin—half from healthy mice and half from mice injected with a fragment of a human melanoma tumor. After a 15 minute application, the ExoPatch was placed under a powerful microscope.
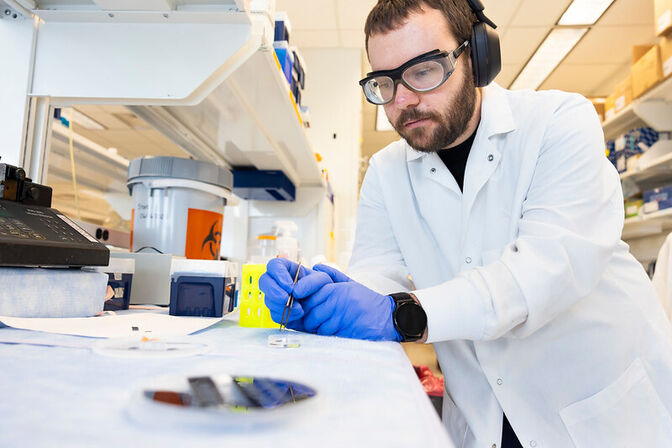
“When looking at microscopy images, I was happy to see how nicely the exosomes adhered to the microneedles and were within the 30 to 150 nanometer size range we expect,” said Scott Smith, a U-M doctoral student of chemical engineering and co-lead author of the study.
After confirming the exosomes stuck to the ExoPatch, the researchers dissolved the gel and ran the sample through the test strips. The test successfully distinguished between melanoma and healthy tissues with a 3.5-fold darker line in melanoma samples.
The ExoPatch isolated 11.5 times more exosomal protein from melanoma tissue samples compared to healthy tissue, showing it can specifically target cancerous exosomes.
A pilot study in humans followed by a series of clinical trials will be the next steps to move the technology toward use. Beyond melanoma, the ExoPatch gel coating could be modified to detect exosomes released by other cancers with a solid tumor—including lung, breast, colon, prostate and brain cancer.
“This is the first patch designed to capture disease-specific exosomes from fluid under the skin. The potential applications are huge,” said Nagrath.
The research is funded by the National Institutes of Health (1-R01-CA-208335-01-A1).
The device was built in the Lurie Nanofabrication Facility and testing was done in part in the Biomedical Research Core Facilities and Rogel Cancer Center Immunology Core.
The team has applied for patent protection with the assistance of U-M Innovation Partnerships.